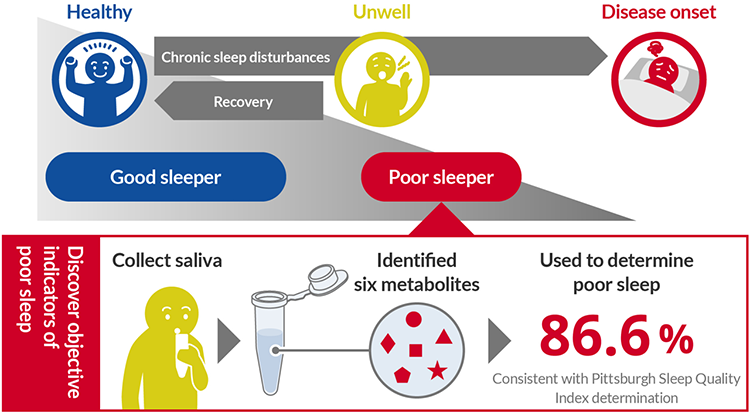
―Machine learning identifies six metabolites to determine chronic poor sleep with 86.6% accuracy―
Researchers) OISHI Katsutaka, Chief Senior Researcher, Cellular and Molecular Biotechnology Research Institute, KAIDA Kosuke, Senior Researcher, Human Informatics and Interaction Research Institute
- Six metabolites in saliva found to be indicators of chronic poor sleep
- The result of Pittsburgh Sleep Quality Index and the assessment of poor sleep based on metabolites in saliva agreed with 86.6% consistency.
- Non-invasive determination is possible and expected to be applied to health care at home, at work, and in elderly care facilities.
Development of non-invasive biomarkers to determine chronic poor sleep
Researchers at AIST, in collaboration with Ibaraki University, have developed a technique to determine chronic poor sleep using saliva.
Sleep disorders are known to increase the risk of developing psychiatric disorders such as depression and lifestyle-related diseases. However, while daily sleep conditions can be measured objectively with relative ease using simple devices, the diagnosis of chronic sleep disorders is difficult, and methods such as the Pittsburgh Sleep Quality Index (PSQI) and sleep diaries rely mainly on the subjectivity of the examinee.
In order to search for non-invasive biomarkers to determine chronic poor sleep, we collected saliva from 50 subjects with no sleep problems with a PSQI score of 2 or less and 50 subjects with poor sleep with a PSQI score of 6 or more and conducted metabolome analysis using CE-FTMS. Based on the concentration information of 683 metabolites that could be detected in the saliva, Random Forest Analysis (a form of machine learning) was conducted to identify six metabolites that are important for discriminating between subjects with no sleep problems and those with poor sleep. Using these, we created a discrimination model and found that we were able to discriminate between those with poor sleep as determined by PSQI scores with consistency of 86.6%.
This achievement not only enables objective and non-invasive evaluation of chronic poor sleep but also has the potential to evaluate changes in daily sleep status, which is considered difficult with the PSQI. In the future, reagent kits and simple devices for measuring metabolites that serve as biomarkers will be developed and established as a self-care technology for sleep, which will be used to monitor the quality of sleep in daily life and for health management at home, at work, and in facilities for the elderly.
Sleep is becoming a growing social concern as society faces issues of 24-hour operations and an aging population. In Japan, it is estimated that one in five adults is not satisfied with their sleep. Sleep disorders are a general term for various disorders related to sleep and wakefulness, and chronic sleep disorders are known to increase the risk of developing psychiatric disorders such as depression, and lifestyle-related diseases. Recently, it has become possible to easily measure daily sleep duration and sleep quality using commercially available wearable devices. However, there are large individual differences in the amount and quality of sleep perceived as satisfactory, and it is necessary to evaluate the long-term sleep status of each individual to assess chronic sleep disorders. Currently, the main methods for evaluating long-term sleep status are self-assessment that relies on the subjectivity of the examinee, such as questionnaires like the PSQI and sleep diaries.
The PSQI is one of the questionnaires used by physicians for diagnosis and screening to evaluate sleep disorders, in which the examinee himself/herself completes a subjective evaluation of 7 items such as sleep quality and sleep duration during the past month, and difficulty in waking up during the day. The total score (0 to 21 points) is used to determine the degree of sleep disturbance. The PSQI is used around the world with a lot of evidence, but there are some problems: the results are dependent on the subjectivity of the examinee, so there is a certain bias, and it is difficult to obtain changes over time. Therefore, it is currently difficult to objectively evaluate chronic poor sleep that may lead to the onset of diseases such as depression.
Journal: Scientific Reports
Title of paper: Potential non-invasive biomarkers of chronic sleep disorders identified by salivary metabolomic profiling among middle-aged Japanese men
Authors: Katsutaka Oishi, Yuta Yoshida, Kosuke Kaida, Kozue Terai, Hiroyuki Yamamoto, Atsushi Toyoda
DOI: 10.1038/s41598-025-95403-1